6 Things to Keep in Mind When Trying to Create a Balanced Mast Cell Activation Diet

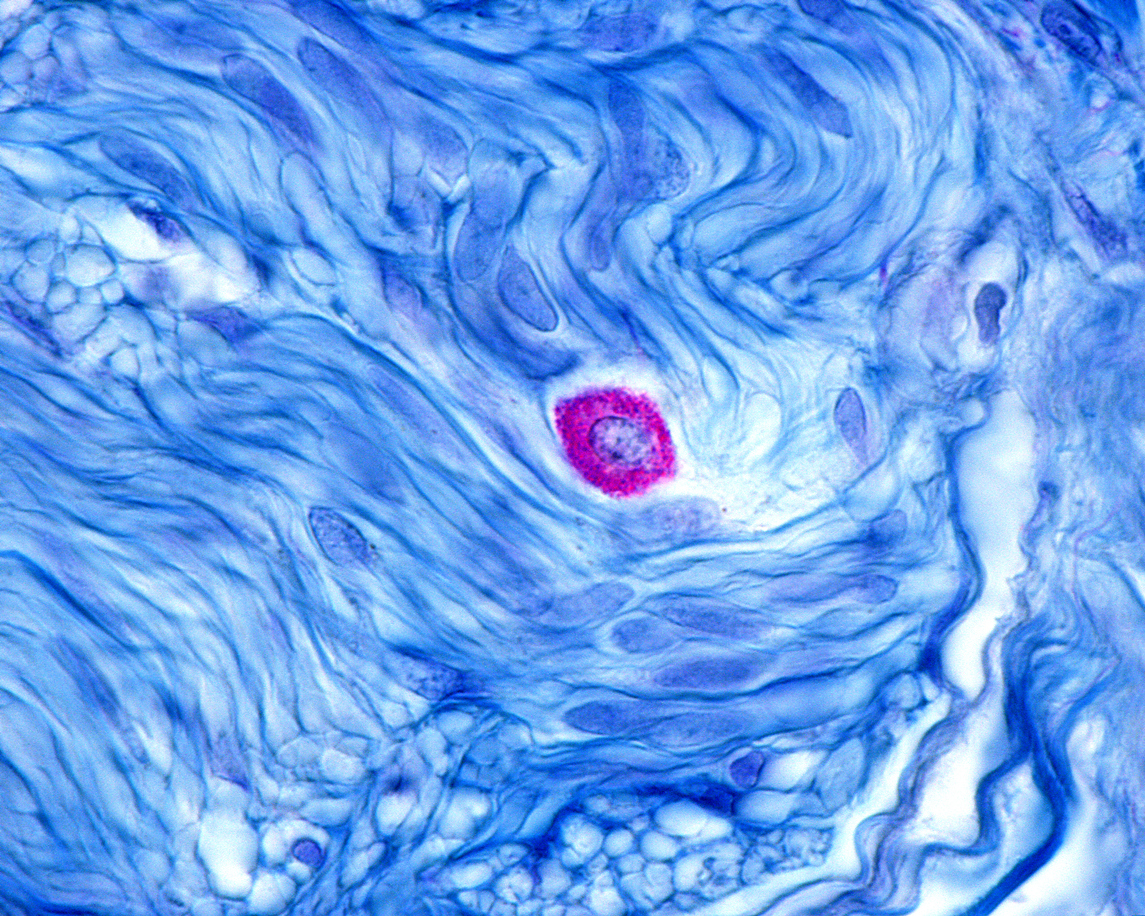
Recognition of mast cell activation disorder (MCAD), a condition in which there is a chronic reactivation of a population of immune cells called mast cells, emerged in the 1980s, with recognition of the condition vastly expanding in recent years. (1) Mast cells are immune cells that release histamine and other pro-inflammatory mediators and play critical roles in regulating the body’s defenses against allergens and pathogens. However, in mast cell activation syndrome (MCAS), mast cell activity goes haywire, causing many symptoms ranging from rashes to fatigue. While the resolution of MCAS is contingent on addressing the underlying causes of the condition, a topic that Chris has previously discussed, diet can play a significant role in quelling MCAS symptoms and supporting recovery. Read on to learn how dietary changes can calm aberrant mast cells and address underlying features of MCAS, supporting a sustainable recovery.
What you should know about MCAS and diet? Read this article from nutritionist Lindsay Christensen to find out. #nutrition #optimalhealth #wellness #mcas
What Is MCAS, and How Is It Affected by Diet?
A mast cell is a type of white blood cell that releases histamine and other pro-inflammatory mediators, such as leukotrienes, cytokines, chemokines, and proteases, to defend the body against pathogens and other environmental stressors such as allergens. (2) Mast cells thus play a vital role in regulating the health and integrity of the tissue microenvironment. However, mast cells can become hyperactive in some individuals, secreting mediators willy-nilly; for example, aberrant mast cell activity is involved in atopy, including asthma and allergies. However, in recent decades, it has become apparent that these conditions are but two examples of aberrant mast cell activity. Mast cell activity can also go haywire inMCAS.
According to MCAS experts Dr. Lawrence B. Afrin, Dr. Mary B. Ackerley, Dr. Joseph H. Brewer, and colleagues in a consensus statement on the condition, up to 17 percent of the general population may have MCAS. (3) In contrast to mastocytosis, a condition characterized by marked neoplasia of mast cells, MCAS is characterized by excessive reactive activation of mast cells.
Several factors may precipitate MCAS, a topic that Chris previously covered in his article “Could Your Histamine Intolerance Really Be Mast Cell Activation Disorder?”, including heavy metals exposure, chronic infections, and gut dysbiosis. Interestingly, Borrelia burgdorferi, the bacterium that causes Lyme disease, (4) or mycotoxin exposure in water-damaged buildings may also activate mast cells. (5)
The gut harbors the largest population of mast cells in the entire body. (6) Mast cells react strongly to external stimuli (such as foods and allergens) and internal stimuli (such as gut bacteria). Based on these lines of evidence, it stands to reason that the foods we eat, which profoundly impact our gut health, will influence mast cell activity. Diet is a powerful tool that can calm aberrant mast cell activity and support healing, alongside medical treatments that address the underlying causes of MCAS. What should you do diet-wise to support MCAS recovery? Let’s talk first about the foods that you should avoid to regulate healthy mast cell activity.
6 Tips That Can Help to Create and Maintain a Good MCAS Diet:
1. Avoid Foods That Trigger Mast Cells
To regulate mast cell activity, it is crucial to first eliminate foods from the diet that trigger aberrant mast cell activity. In my clinical experience, the foods that most consistently trigger mast cell activity include:
- Industrial seed oils: Chris has previously written about the harmful health effects of consuming industrial seed oils. Industrial seed oils, including canola, corn, cottonseed, grape seed, safflower, soybean, and sunflower oils, are rich in omega-6 fatty acids. In preclinical research, a high intake of soybean oil is associated with an enhanced mast cell response. (7) The oxidized lipids found in vegetable oils trigger a chain reaction of oxidative stress in the body (8); oxidative stress can, in turn, activate mast cells. (9) To calm hyperactive mast cells, remove unhealthy vegetable oils from your diet, and instead focus on eating anti-inflammatory fats, such as extra virgin olive oil and coconut oil.
- Food additives: In my clinical experience, I’ve found that food additives such as carrageenan, sodium benzoate, potassium sorbate, maltodextrin, MSG, smoke flavoring, yeast extract, and citric acid can activate mast cells in sensitive individuals. The good news is that you can easily avoid many of these additives by eschewing processed foods and switching to a whole-food, anti-inflammatory diet.
- Processed foods: Processed foods should be avoided by people with MCAS because such foods tend to contain industrial seed oils, food additives, and refined carbohydrates that trigger mast cells, perpetuate gut microbiota disruption, and contribute to ongoing immune system imbalances. (10)
- Pesticide- and herbicide-exposed foods: Research indicates that the herbicide glyphosate, which widely contaminates our food supply, induces the expression of interleukin 33 (IL-33), an immune signaling molecule involved in T helper type 2 (Th2) allergy-oriented immune responses. IL-33 augments the effect of immunoglobulin E (IgE) on the secretion of histamine from mast cells, suggesting that glyphosate exposure may be a trigger for mast cell activity. (11) Choose organic foods as often as your budget allows, or refer to the Environmental Working Group’s Dirty Dozen list to prioritize which foods to purchase organic.
In addition to avoiding industrial seed oils, food additives, processed foods, and foods heavily contaminated with pesticides and herbicides, people with MCAS may also benefit from the following:
2. Limit Antinutrient Intake
Many antinutrients, such as phytic acid and oxalate, increase intestinal permeability, aka “leaky gut.” Increased intestinal permeability facilitates mast cell activation. (12) While strict avoidance of dietary antinutrients is not necessarily realistic or ideal, you may want to avoid foods that are exceptionally high in antinutrients or prepare foods in ways that reduce their antinutrient content. For example, you may want to limit your consumption of grains, which contain large amounts of the antinutrients phytic acid/phytate, lectins, and saponins. Legumes are also high in lectins. If you are really struggling with MCAS, you might consider going grain- and legume-free for a period. Alternatively, you can soak grains and legumes before cooking them to reduce their antinutrient content. Other sources of antinutrients to consider include foods high in oxalate, an antinutrient that binds dietary calcium. High-oxalate foods include spinach, beets, and chocolate.
3. Consider Assessing for Food Allergies and Sensitivities
In a true food allergy, a food-based molecule called an antigen triggers the body to make an IgE antibody, a blood protein created to counteract the antigen. The IgE antibody incites mast cells to “degranulate,” releasing histamine and other pro-inflammatory mediators. Avoiding foods to which one is allergic is thus crucial for mitigating mast cell activation. While those with food allergies typically need to avoid specific foods for life, immunotherapies such as sublingual immunotherapy may help some individuals desensitize themselves to food allergens. (13)
Another more controversial but potentially helpful consideration is to assess for immunoglobulin G (IgG)-mediated food sensitivities while understanding the limitations. Unlike a food allergy, which is mediated by IgE antibodies, IgG antibodies have been considered in the Functional Medicine space to indicate a delayed hypersensitivity response to a food. While certain authorities, including the American Academy of Allergy, Asthma & Immunology, argue that IgG food sensitivity tests are useless (14), the truth is likely more nuanced. High levels of IgG antibodies to specific foods in the blood may simply reflect heavy consumption of the food in the individual’s diet; however, IgG reactions to foods are both a cause and a result of increased intestinal permeability. Therefore, IgG food sensitivity is not necessarily a long-term problem and may be resolved by improving gut health. However, in the short term, people with strong IgG food sensitivities may benefit from avoiding the foods to which they are sensitive to limit further damage to the intestinal barrier.
4. Consider Whether Histamine Sensitivity Is an Issue
Mast cells release copious amounts of histamine, increasing the body’s endogenous histamine burden. The consumption of high-histamine foods, such as fermented foods, will further contribute to the body’s histamine burden and may thus exacerbate symptoms in those with MCAS. In my clinical experience, not all people with MCAS appear to be sensitive to high-histamine foods, perhaps because histamine is not the only inflammatory mediator released by mast cells. However, many people with MCAS do experience reactions to high-histamine foods and may benefit from eating largely lower-histamine foods.
5. Consider Gluten Sensitivity Testing
Gluten is a common dietary inflammatory trigger that activates mast cells and disrupts the intestinal barrier, potentially initiating and perpetuating mast cell hyperreactivity. Mast cell-nerve interactions appear to relate to bloating and abdominal pain in patients with non-celiac gluten sensitivity (15); furthermore, gluten peptides can bind to Toll-like receptors on mast cells, sensitizing mast cells and causing them to release pro-inflammatory cytokines. (16) For those with MCAS who are not already avoiding gluten, gluten sensitivity testing will help determine whether gluten avoidance is necessary. Your practitioner can use a test such as Cyrex Array 3 to assess for gluten sensitivity.
6. How to Eat to Promote Balanced Mast Cell Activity
The best diet for balancing mast cell activity is anti-inflammatory, nutrient-dense, and centered around real foods. It sounds a lot like a Paleo diet, right? I have found a Paleo template diet that makes concessions for patients’ unique dietary triggers works very well for calming mast cell activity, repairing gut health, and reducing symptoms. A mast cell-stabilizing diet should be centered around the following foods:
- Choose high-quality proteins, such as grass-fed beef, organic and pastured poultry, and wild-caught seafood. If you are histamine-sensitive, stick with the freshest meats and seafood you can find, and avoid cured meats and smoked fish.
- Eat a wide variety of fresh organic vegetables and fruits to optimize your intake of antihistamine phytonutrients, such as quercetin and sulforaphane (17), and provide your gut bacteria with ample dietary fiber to make the short-chain fatty acid butyrate, a compound with mast cell-stabilizing activity. (18) The consumption of at least 25 grams of fiber per day may be ideal.
- Consume anti-inflammatory fats, with a particular focus on the omega-3 fatty acids EPA and DHA. These essential fatty acids stabilize mast cells, regulating overall immune function. (19)
- Optimize your intakes of vitamins A, D, E, and C, which regulate immune function. Vitamin D, in particular, stabilizes mast cells, while vitamin C offers antihistamine effects. (20, 21, 22)
- Incorporate functional foods with mast cell-stabilizing properties, such as pomegranate, onion, capers, moringa, nettle, and Thai ginger (galangal).
When you eat may be just as important as what you eat as far as mast cells are concerned. Research indicates that mast cell activity is tightly linked to our circadian rhythms, the patterns of behavioral and physiological changes that occur in our bodies on a roughly 24-hour schedule. Eating in a manner aligned with the light/dark cycle, eating primarily during daylight hours, and limiting food consumption at night may provide further support for balanced mast cell activity. (23)
MCAD is tricky, but eating well can do wonders for quelling symptoms and supporting healing. If you’ve dealt with MCAD, I’d love to hear about the strategies that have helped you!






